Primary gastrointestinal mantle lymphoma with massive bleeding: a case report and literature review
Introduction
Primary gastrointestinal lymphomas (PGILs) originate in the gastrointestinal tract, with or without the other parts of the lymph nodes or the presence of lymphatic tissue invasion (1). The incidence of lymphomas has increased steadily within the last 10 years. PGIL is the most common extranodal lymphoma, accounting for 5% to 20% of all lymphomas and about 1% to 4% of all gastric malignancies. The most commonly involved site is the stomach, followed by the small intestine and the ileocecal region (2). The most common histologic subtypes are diffuse large B cell lymphomas (47%) and marginal zone B cell lymphomas (24%), with very few mantle lymphomas (5%) (3).
A standard treatment regimen has not been established for PGIL. Less life-threatening gastrointestinal bleeding occurs after chemotherapy and few reports about the bleeding of primary gastrointestinal mantle lymphomas have been published. In the last 10 years, rituximab was found to improve the clinical outcome of patients with B cell malignancies. In this case, the severe gastrointestinal bleeding was caused by low-dose chemotherapy, which was dramatically improved by rituximab monotherapy. Therefore, we discussed the treatment options with a brief review of the literature.
Case report
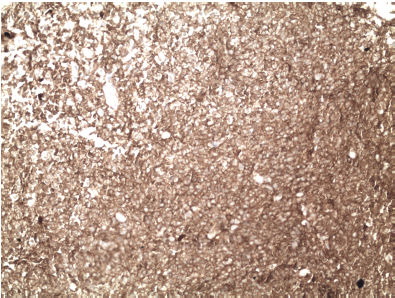
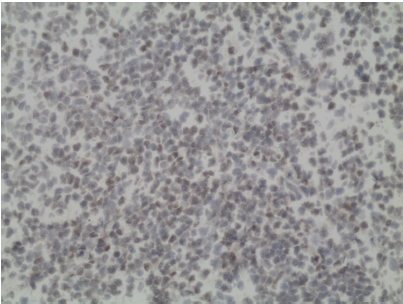
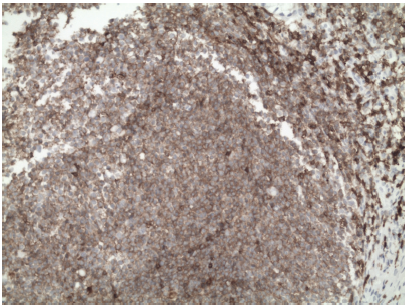
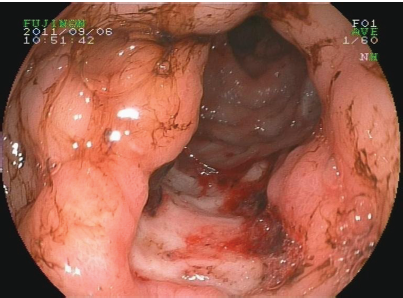
A 73-year-old male with an 8-month history of intermittent bloody stool, dizziness and sweating was admitted to Peking University Cancer Hospital. The patient suffered from an acute myocardial infarction in 1983. Multiple enlarged cervical lymph nodes were found bilaterally in the physical examination, without hepatosplenomegaly and abdominal mass. Blood analysis showed anemia (hemoglobin at 66 g/L), with normal white blood counts, platelet count, and coagulation parameters. His serum biochemistry profiles, including liver enzymes, renal function, and lactate dehydrogenase (LDH), were within normal limits. Computed tomography (CT) of the thorax and pelvic ultrasound were performed; all findings were within the normal range. Abdominal ultrasound revealed an upper abdominal mass measuring 9.1 cm × 4.8 cm. The upper gastroscopy showed a large amount of fresh blood with multiple gastric ulcers. The largest ulcer, located in the anterior pyloric wall, measured 3 cm × 1.5 cm. Gastroscopy showed multiple nodular lesions in the gastric cavity (Figure 1). Histopathologic examination of biopsies from the gastric lesions demonstrated mantle cell lymphoma. Under immunohistochemical staining, the tumor cells were positive for CD20, PAX5, CD5, cyclin D1, CD68, Bcl-2 and Ki-67 (40%), and negative for cytokeratin (CK), epithelial membrane antigen (EMA), CD23, CD10 and Bcl-6 (Figures 2-4). Colonoscopy confirmed the results of the gastroscopy. Bone marrow aspiration biopsy showed typical lymphocytic infiltration. The patient developed massive digestive tract hemorrhage, bright red hematemesis, melena, and hemorrhagic shock during low-dose combination chemotherapy consisting of cyclophosphamide (200 mg on d1 and d2) and vindesine (1 mg on d1 and d2). The patient was given blood transfusions, hemostasis, fasting, and acid suppression. Intravenous rituximab monotherapy was administered thrice (600 mg). The melena gradually improved to normal yellow stools, and hemoglobin increased to 110 g/L. Follow-up gastroscopy showed significant improvement, and the large pyloric ulcer disappeared. The patient was administered with R-CHOP chemotherapy every 3 weeks. The therapy consisted of rituximab (600 mg on d1), cyclophosphamide (200 mg on d2 and d3), doxorubicin (20 mg on d2 and d3), and vincristine (0.5 mg from d2 to d4). Follow-up CT scan of the abdomen after six cycles of R-CHOP chemotherapy showed that the previous abdominal masses nearly disappeared. Bone marrow aspiration biopsy was negative for lymphocytic infiltration.
Discussion
PGIL is difficult to distinguish from other gastrointestinal tumors, and its treatment is apparently different. The main clinical symptoms are abdominal pain, abdominal mass, changes in bowel habits, obstruction, and bleeding. The patient manifested recurrent gastrointestinal bleeding and severe anemia, and was eventually diagnosed as mantle cell lymphoma.
The PGIL examination included gastrointestinal barium swallow, abdominal CT, positron emission tomography-computed tomography (PET-CT), and endoscopy. The manifestations of PGIL are as follows: (I) Submucosal nodules were single or multiple, or coalesced into a larger mass. (II) Differently sized ulcer can be found on the surfaces of the masses. Endoscopy showed irregular ulcers, mucosal edema, destruction, necrosis, and hyperplastic nodules. Pathologic examination confirmed the diagnosis of PGIL.
The various therapeutic regimens for PGIL, including rituximab, chemotherapy, radiotherapy and surgical treatment, are still controversial. Avils (4) reported a controlled clinical trial. Up to 589 patients were randomized to receive any of the following therapeutic approaches: surgery, surgery + radiotherapy, surgery + chemotherapy, and chemotherapy. The complete response (CR) rates were similar in the four treatments, but the 10-year overall survival (OS) rates revealed statistically significant improvements in chemotherapy (96%) and surgery + chemotherapy (91%). Surgery and surgery + radiotherapy were associated with poor prognosis. Cheung et al. (5) evaluated the effects of surgery on gastrointestinal lymphomas. A total of 17,222 cases were included in the meta-analysis. In the univariate analysis, surgical excision did not improve survival. Rituximab revolutionized the treatment strategies for patients with B cell lymphoma over the last decade. The addition of rituximab to CHOP chemotherapy significantly improved the prognosis and survival of patients with diffuse large B cell lymphomas (6). The CR was 95% and 5-year OS of stage IE and IIE PGIL is 95% (7). We reported the case of mantle cell lymphoma involving the gastrointestinal tract. The severe gastrointestinal bleeding was caused by low-dose chemotherapy, which was controlled with rituximab monotherapy. The combination of rituximab with chemotherapy was continued.
Gastrointestinal lymphomas are different from other types of lymphoma. Gastrointestinal lymphoma can develop gastrointestinal bleeding, perforation, and life-threatening hemorrhage during chemotherapy (8). The incidence of bleeding among patients receiving chemotherapy is up to 11% (9). Therefore, we firstly need to confirm gastrointestinal ulcer and bleeding before chemotherapy. When large ulcers or ulcers near great vessels are present, chemotherapy should be performed after the operation. Secondly, chemotherapy should be initiated at low doses to avoid rapid tumor necrosis and hemorrhage. Thirdly, we need to reduce the amount of hormones. Finally, doctors should inform the patients about the manifestations of gastrointestinal bleeding.
Systemic therapy is the treatment of choice, whereas surgery selection is only indicated for those with obstruction, perforation, and bleeding (10,11).
In summary, primary gastrointestinal mantle lymphomas can develop life-threatening gastrointestinal bleeding after chemotherapy. The prevention and treatment of gastrointestinal bleeding of PGIL should be given much attention. The therapeutic approach for PGIL is still controversial. Our data provide evidence that rituximab is safe and effective for gastrointestinal mantle cell lymphomas. Older and weaker patients can be successfully treated with rituximab monotherapy. Younger patients should be given standard immunochemotherapy, which includes rituximab and cytarabine-based regimens (12).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg 1961;49:80-9.
- Ghimire P, Wu GY, Zhu L. Primary gastrointestinal lymphoma. World J Gastroenterol 2011;17:697-707.
- Howell JM, Auer-Grzesiak I, Zhang J, et al. Increasing incidence rates, distribution and histological characteristics of primary gastrointestinal non-Hodgkin lymphoma in a North American population. Can J Gastroenterol 2012;26:452-6.
- Avilés A, Nambo MJ, Neri N, et al. The role of surgery in primary gastric lymphoma: results of a controlled clinical trial. Ann Surg 2004;240:44-50.
- Cheung MC, Housri N, Ogilvie MP, et al. Surgery does not adversely affect survival in primary gastrointestinal lymphoma. J Surg Oncol 2009;100:59-64.
- Coiffier B, Lepage E, Briere J, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 2002;346:235-42.
- Avilés A, Castañeda C, Cleto S, et al. Rituximab and chemotherapy in primary gastric lymphoma. Cancer Biother Radiopharm 2009;24:25-8.
- Shum JB, Jayaraman S, Croome K, et al. Upper gastrointestinal and intra-abdominal hemorrhage secondary to diffuse large B-cell gastric lymphoma. Can J Surg 2008;51:E56-7.
- Velicković D, Sabljak P, Ebrahimi K, et al. Upper gastrointestinal bleeding as a surgical complication of primary gastric lymphoma. Acta Chir Iugosl 2007;54:131-4.
- Chao TC, Chao HH, Jan YY, et al. Perforation through small bowel malignant tumors. J Gastrointest Surg 2005;9:430-5.
- Zheng W, Zhu J, Yong WB, et al. Non-Hodgkin’s lymphoma with gastrointestinal perforation: report of 8 cases. Shi Yong Ai Zheng Za Zhi 2007;22:503-5.
- Delarue R, Haioun C, Ribrag V, et al. CHOP and DHAP plus rituximab followed by autologous stem cell transplantation (ASCT) in mantle cell lymphoma (MCL): a phase II study from the GELA. Blood 2013;121:48-53.