Value of 18F-FDG PET/CT and MRI in diagnosing primary endometrial small cell carcinoma
Introduction
Primary small cell carcinoma (SCC) is a group of aggressive neoplasms that mainly arise from the lung and digestive tract. It could affect almost any organ such as the ampulla of Vater, gallbladder, ovary, sphenoid sinus, Meckel’s diverticulum, epiglottis, genitourinary tract, etc. (1,2). In the female genital tract, it occurs most commonly in the cervix (3). SCC in the endometrium is extremely rare and comprises less than 1-2% of all malignant gynecologic tumors (4). Herein, we present a new endometrial small cell carcinoma (ESCC) case involving a 51-year-old woman. To our knowledge, less than 90 cases have been reported until now. Moreover, few magnetic resonance imaging (MRI) and 18F-fludeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) findings for ESCC have been reported in English literature. This report mainly focuses on the MRI and PET/CT presentations of ESCC.
Case report
A 51-year-old woman was admitted to the Department of Gynecology because of irregular postmenopausal bleeding for 2 months. The quantity of blood was variable. A large quantity was always associated with abdominal pain, abdominal distention, urinary frequency, and urinary urgency. Immunohistochemical studies revealed a neoplasm with neuroendocrine characteristics. The tumor cells demonstrated a positive reaction with markers vimentin (VIM), synaptophysin (Syn), neuron-specific enolase (NSE), CD99, CD10, and epithelial membrane antigen (EMA), as well as a high Ki67 proliferation rate (about 50% positive cells), but stained negatively for chromogranin A (CgA), cytokeratin (CK), cyclin D1, LCA, CD31, estrogen receptor (ER), progestin receptor (PR), human melanoma black-45 (HMB45), CD117, inhibin, CD56, CD34, CD3, CD20, myeloperoxidase (MPO), and S-100.
An MRI showed that the uterus was significantly enlarged (11.6 cm × 11.1 cm × 14.4 cm), and a giant irregular mass (7.5 cm × 8.4 cm × 8.5 cm) was observed in the uterus cavity. The mass demonstrated heterogeneously low signal intensity on T1-weighted imaging (Figure 1A) and slightly high signal intensity on T2-weighted fat-suppressed spectral presaturation attenuated inversion-recovery (SPAIR) (Figure 1B). The lesion showed a high signal intensity on diffusion-weighted imaging (DWI) (b=800 s/mm2) (Figure 1C) and a low signal intensity on apparent diffusion coefficient (ADC) map (Figure 1D). The ADC value was (0.553±0.088)×10–3 mm2/s. Sagittal T1-weighted contrast-enhanced fat-suppressed imaging (Figure 1E) showed a non-homogeneously enhanced entity, and an unenhanced area was found in the mass. It also revealed deep myometrial (>50%) invasion, as well as infringement of the cervix and vagina.

PET/CT imaging (Figure 2) demonstrated a large solid mass in the uterine cavity. Uterine enlargement and cervical invasion were also revealed. Multiple metastatic lymph nodes (LNs) (diameter range, 0.3-2.8 cm) have been identified at different positions: left supraclavicle [the maximum standardized uptake value (SUVmax) =15.5], mediastinum (SUVmax range, 7.6-11), right lower abdomen (SUVmax =15.7), and post-peritoneum (SUVmax range, 6.9-19.3). The SUVmax of the primary lesion was 22.7. The pelvic and bilateral inguinal LNs showed no obvious enlargement or FDG uptake.

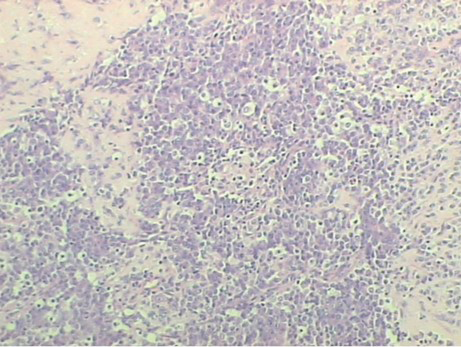
The patient underwent surgery including panhysterocolpectomy, bilateral salpingo-ovariectomy, and primary cytoreductive surgery. A macroscopic examination of the uterus revealed a bulky mass that almost completely infiltrated the myometrial wall (Figure 3). The postoperative stage was defined as stage IVB. Endometrial biopsy specimens showed that the uterine tumor tissue was saturated with atypical cells including auxetic nuclei (Figure 4).
A relapse was confirmed 6 months later. An MRI revealed multiple nodules on remaining vaginal wall and enlarged pelvic LNs.
Discussion
Primary SCC is rare, comprising less than 1-2% of all malignant gynecologic tumors (4). According to the studies reported in prior reviews and case reports (5-7), the age at presentation ranges from 23 to 84 years, with a mean age of approximately 60 years, and is higher than that of endometrial adenocarcinomas, which is 50 years.
The most frequent clinical presentation is abnormal vaginal bleeding. Other complaints include lower abdominal or pelvic pain and irregular menstruation. All of these presentations are nonspecific for determining a diagnosis. Thus, Van Hoeven et al. (7) proposed the diagnostic criteria for SCC of the endometrium: (I) unequivocal evidence of endometrial origin; (II) dense sheet-like growths of morphologically similar, small to intermediate-sized tumor cells in standard hematoxylin-eosin (HE)-stained sections; and (III) immunohistochemical staining for one or more neuroendocrine markers. Katahira et al. (6) reported summarized data based on reported cases: SCC of the endometrium is typically positive for NSE (79%), Leu-7 (61%), Syn (42%), and CgA (38%).
Similarities regarding the histopathology and immunohistochemistry of SCC from different positions have already been recognized. This kind of neoplasm behaves in an aggressive manner including early involvement of LNs. Yang et al. (8) reported that SCC of the cervix is characterized by extensive lymphadenopathy (which means one or several LNs conglomerated together with a minimum diameter of >1 cm). Even a small mass (<4 cm) has a considerable chance of LN involvement. From what we can infer, ESCC might have similar biological behaviors and imaging features. Because of the limited number of cases, this perspective needs to be further confirmed.
The prognosis of small cell neuroendocrine carcinoma (SCNEC) is extremely poor. Based on present data, the prognosis is closely related to stage. Among the known stage I cases, most patients have a better prognosis. Some even lived for 5 years or more with no evidence of disease. Stage III and IV patients had an average survival of only 5 months. Thus, detection at an early stage plays a vital role in patients’ long-term survival.
PET/CT has poor efficacy for the detection of early lesions (<1 cm) in the uterus because of its limited spatial resolution. Additionally, because of this reason, it is hard for radiologists to accurately measure the local extent of uterine body invasion with PET/CT scanning. However, quite a few studies have shown that the SUVmax is a prognostic factor in endometrial cancer. In this case, the SUVmax of the primary lesion (22.6) was high. Although this value cannot help in differentiating the entity from conventional adenocarcinoma, it indicated a poor prognosis. The superiority of PET/CT also depends on its facility for helping to discover the involvement of tiny LNs (minimum diameter, >0.5 cm) (9) and retroperitoneal LN and distant metastases, which is significant for staging and therapeutic scheduling. In this case, the minimum diameter of the metastatic LN was 0.3 cm, which was smaller than previously reported. This helps define the ability of PET/CT for detecting small lesions. In addition, a recent study (10) found that the preoperative FDG uptake of a pelvic LN exhibited a strong significant association with recurrence of endometrial cancer. Recurrence rates differed significantly (P<0.001) between patients with an SUVLN >15 and those with an SUVLN ≤15. However, in this case, pelvic LNs demonstrated no obvious enlargement or FDG uptake. Instead, an SUVLN >15 was demonstrated at three different distant locations. Recurrence was confirmed 6 months later. This is slightly different from the previous study but still indicated that LN metabolic activity may reflect tumor aggressiveness and a poor prognosis.
MRI provides valuable and important information regarding lesion location, as well as qualitative information and preoperative staging. Because of the lack of literature, the MRI features of ESCC are not clear. In this case, the lesion was a bulky mass with slightly low signal intensity on T1-weighted imaging and had heterogeneous high signal intensity on T2-weighted imaging. T1 contrast-enhanced fat-suppressed imaging demonstrated uneven enhancement of the tumor and junctional zone disruption, which is a significant marker for myometrial infiltration. On a routine MRI scan, SCC may differ from typical adenocarcinomas in respects of larger shape, vascularity, and higher tendency for necrosis.
The ADC value of this lesion (solid part) was (0.553±0.088)×10–3 mm2/s, which was much lower than (1.011±0.121)×10–3 mm2/s that was the mean ADC value of endometrial non-SCC according to a large case observation (11). However, we cannot simply reach a conclusion regarding the ADC value related to the histological type, as the difference is probably because of different MRI manufacturers, a different selected b value, and region-of-interest (ROI) drawing method. Thus, this perspective still necessitates confirmation with further research. Both ovaries demonstrated a high intensity with DWI, and the ADC value was (0.711±0.069)×10–3 mm2/s, which suggested ovarian metastases. This was confirmed by PET/CT (on which ovaries demonstrated a high FDG uptake) and pathology. Furthermore, the ADC map revealed the myometrial infiltration more clearly than both conventional MRI and PET/CT. These might indicate that DWI is, on one hand, a sensitive and useful tool for assessing metastases that aids in accurate preoperative staging and appropriate management decision-making, and on the other hand, this technique is radiation-free and not time-consuming, as compared with PET/CT.
In conclusion, we suggest that MRI, along with DWI, can be used as an important and preferred tool to assess ESCC in clinical practice. Confirmation of the additional diagnostic value of DWI is required. PET/CT should be used to detect tiny, distant metastatic LNs. The SUVmax of both a primary lesion and LNs may have great value in predicting prognosis.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Hubalewska-Dydejczyk A, Trofimiuk M, Sowa-Staszczak A, et al. Neuroendocrine tumours of rare location. Endokrynol Pol 2010;61:322-7. [PubMed]
- Lee HY, Wu WJ, Tsai KB, et al. Primary small cell carcinoma of kidney after renal transplantation: a case report and literature review. Chin J Cancer Res 2013;25:608-11. [PubMed]
- Hwang JH, Lee JK, Lee NW, et al. Primary small cell carcinoma of the endometrium: report of a case with immunochemical studies. J Reprod Med 2010;55:81-6. [PubMed]
- Crowder S, Tuller E. Small cell carcinoma of the female genital tract. Semin Oncol 2007;34:57-63. [PubMed]
- Matsumoto H, Takai N, Nasu K, et al. Small cell carcinoma of the endometrium: a report of two cases. J Obstet Gynaecol Res 2011;37:1739-43. [PubMed]
- Katahira A, Akahira J, Niikura H, et al. Small cell carcinoma of the endometrium: report of three cases and literature review. Int J Gynecol Cancer 2004;14:1018-23. [PubMed]
- van Hoeven KH, Hudock JA, Woodruff JM, et al. Small cell neuroendocrine carcinoma of the endometrium. Int J Gynecol Pathol 1995;14:21-9. [PubMed]
- Yang DH, Kim JK, Kim KW, et al. MRI of small cell carcinoma of the uterine cervix with pathologic correlation. AJR Am J Roentgenol 2004;182:1255-8. [PubMed]
- Nogami Y, Iida M, Banno K, et al. Application of FDG-PET in cervical cancer and endometrial cancer: utility and future prospects. Anticancer Res 2014;34:585-92. [PubMed]
- Chung HH, Cheon GJ, Kim HS, et al. Preoperative PET/CT standardized FDG uptake values of pelvic lymph nodes as a significant prognostic factor in patients with endometrial cancer. Eur J Nucl Med Mol Imaging 2014;41:1793-9. [PubMed]
- Cao K, Gao M, Sun YS, et al. Apparent diffusion coefficient of diffusion weighted MRI in endometrial carcinoma-Relationship with local invasiveness. Eur J Radiol 2012;81:1926-30. [PubMed]


